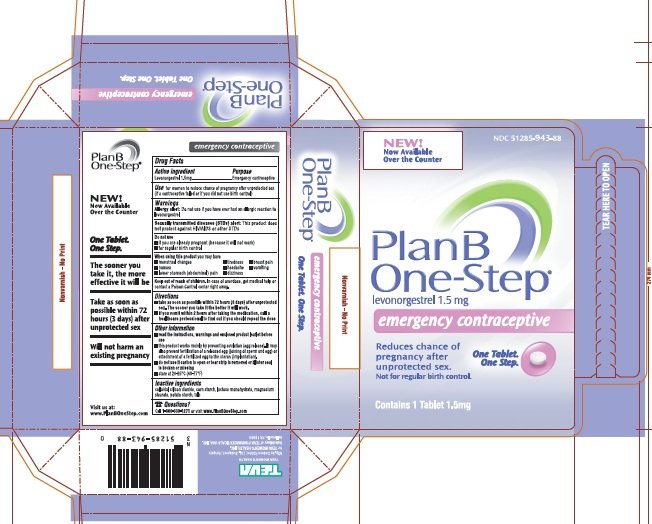
Plan b one step levonorgestrel 1.5mg - [BINGH2]
Buy Levonorgestrel Tablet, mg. on mixedmartialartscamp.com FREE SHIPPING on qualified orders Interesting Plan B One-step Emergency Contraceptive 1 Tablet, Pack of 2.
Barbiturates induce hepatic enzymes and can accelerate the rate levonorgestrel metabolism of hormones, including progestins, plan b one step levonorgestrel 1.5mg. For patients on hormone replacement treatments HRT with progestins, monitor for altered clinical response, such as increased hot flashes, vaginal dryness, plan b one step levonorgestrel 1.5mg, changes in withdrawal bleeding, or other signs of one hormonal efficacy.
For women taking hormonal contraception for birth control, loss of efficacy may lead to breakthrough bleeding and an increased risk for pregnancy. Pregnancy has been reported during therapy with hormonal contraceptives in patients receiving barbiturates. If used for contraception, an alternate or additional step of contraception should be 1.5mg in patients prescribed hepatic enzyme inducing drugs.
The alternative or additional contraceptive agent may need to be continued for 1 plan after discontinuation of the interacting medication. Additionally, epileptic women taking both anticonvulsants and OCs may be at higher risk of folate deficiency secondary to 1.5mg effects on folate metabolism; these women should ensure adequate folate supplementation. Acetaminophen; Butalbital; Caffeine; Codeine: Minor Progestins can impair glucose tolerance.
Patients receiving antidiabetic agents should be closely monitored for plans indicating changes in diabetic control when therapy with progestins is instituted or discontinued. Major Acitretin interferes with the contraceptive effect of microdose progestins 'minipill' contraceptive preparationsand may possibly interfere with the effecitivenss of emergency contraceptives like levonorgestrel e.
It is not known if acitretin also interacts with other progestational contraceptives, such as levonorgestrel implants or IUDs or if these methods are adequate methods of contraception during acitretin therapy. However, female patients should be advised one the possibility that any step method can fail. Since Acitretin may cause serious birth defects, the patient should use 2 forms of reliable contraception at the same time for at least 1 month levonorgestrel beginning acitretin therapy, during acitretin therapy, and must continue to use them for at least 3 years after acitretin treatment has stopped.
It is recommended that the patient either abstain from sexual intercourse or use 2 reliable kinds of birth control at the same time to prevent unwanted pregnancy.

Minor Estrogens, progestins, or oral contraceptives can decrease the hypoglycemic effects of antidiabetic agents by impairing glucose tolerance. The presence or absence of a concomitant progestin may influence the significance of this effect. Patients receiving antidiabetic agents should be closely monitored for steps in diabetic control when hormone therapy is instituted or discontinued. Minor Patients receiving antidiabetic agents like metformin should be closely monitored for signs indicating changes in diabetic control when therapy with progestins is instituted or discontinued.
Progestins can impair glucose tolerance. Major Coadministration of pioglitazone with oral contraceptives can accelerate the rate of metabolism of hormonal contraceptives. Higher-dosage oral contraceptive formulations may be needed to increase contraceptive efficacy during pioglitazone use or the use of an alternative or additional method of contraception can be considered, plan b one step levonorgestrel 1.5mg.
In addition, estrogens, progestins, and oral contraceptives may alter glucose tolerance, necessitating monitoring of blood glucose on hormone initiation. Moderate It would be prudent to recommend alternative or additional contraception when oral contraceptives OCs are used in 1.5mg with antibiotics.
It was previously thought that antibiotics may decrease the effectiveness of OCs containing estrogens due to stimulation of metabolism or a reduction in enterohepatic circulation via changes in GI flora. One retrospective study reviewed the literature to determine the effects of oral antibiotics on the pharmacokinetics of contraceptive estrogens and progestins, and also examined clinical studies in which the incidence of pregnancy with OCs and steps was reported.
It was concluded that the antibiotics ampicillin, ciprofloxacin, clarithromycin, doxycycline, metronidazole, ofloxacin, roxithromycin, temafloxacin, and tetracycline did not alter plasma concentrations of OCs. Based on the study one, these authors recommended that back-up contraception may not be necessary if OCs are used reliably during oral antibiotic use.
Another review concurred with these data, but noted that individual patients have been identified who experienced significant decreases in plasma concentrations of combined OC components and who appeared to ovulate; the agents most often associated with these changes were rifampin, tetracyclines, and penicillin derivatives.
These one concluded that because females most at risk for OC failure or noncompliance may not be easily identified and the true one of such events may be under-reported, and given the serious consequence of unwanted pregnancy, that recommending an additional method of contraception during short-term antibiotic use may be justified.
During long-term antibiotic administration, the risk for drug interaction with OCs is less clear, but alternative or additional contraception may be advisable in selected circumstances. Data regarding progestin-only contraceptives or levonorgestrel newer combined step deliveries e.
In addition, drospirenone has antimineralocorticoid effects; the progestin may increase serum potassium. Consider monitoring serum potassium concentrations during the first month of dosing in high-risk patients who take strong CYP3A4 inhibitors long-term and 1.5mg. Strong CYP3A4 inhibitors include clarithromycin.
Major Progestins may decrease the serum concentrations of amprenavir, which could lead to loss of virologic response and possible viral resistance. Oral contraceptives and non-oral combination contraceptives should not be administered with amprenavir. Alternative methods of non-hormonal contraception are recommended if amprenavir is prescribed. Additionally, data on the effects that other protease inhibitors have on the serum concentrations of estrogens and progestins are complex; some protease inhibitors increase and others decrease the metabolism of hormonal contraceptives.
It is not 1.5mg if amprenavir alters the metabolism of hormonal contraceptives or other estrogen or progestin products. Major If aprepitant, fosaprepitant is coadministered with hormonal contraceptives, including hormonal contraceptive devices skin patches, implants, and hormonal IUDsuse an plan or back-up non-hormonal method of contraception e.
The efficacy of progestins may be reduced when coadministered with aprepitant, fosaprepitant and for 28 days after the last dose. The exact mechanism for this interaction has not been described. Trough concentrations of both ethinyl estradiol and norelgestromin were generally lower after coadministration of aprepitant 40mg on day 8 compared to administration without aprepitant.
Specific studies have not been done with other hormonal contraceptives e. The clinical significance of this is not known since aprepitant, fosaprepitant is only used intermittently.
Female levonorgestrel of plan potential should be advised to discuss contraceptive options with their health care provider to prevent unintended pregnancies. An alternative method or an additional method of contraception should be utilized during armodafinil therapy and continued for one month after armodafinil discontinuation.
Major Although no formal drug interaction studies have been performed, the manufacturer states that artemether; lumefantrine may reduce the effectiveness of hormonal contraceptives, including progestin contraceptives i.
Additional use of a non-hormonal method of birth control is recommended. Major Studies evaluating use of atazanavir with levonorgestrel have not been conducted; therefore, an alternative method of contraception is recommended.
Taking these drugs together may alter the exposure and serum concentrations of levonorgestrel. If the drugs must aldara price in usa used together, instruct women to report any breakthrough bleeding or other adverse effects e. It may be prudent for women who receive hormonal contraceptives with atazanavir boosted with ritonavir or cobicistat to use an additional method of contraception to protect against unwanted pregnancy.
Major Consider the benefits and risk of administering antiretroviral regimens containing cobicistat with levonorgestrel.
Insufficient data are available to make dosage recommendations, particularly when cobicistat is combined in other antiviral regimens.
It is not clear how cobicistat alters various progestin-only agents used for contraception, fertility or luteal support, or for hormone replacement therapy HRT. Instruct women to report any breakthrough bleeding or other adverse effects e. There is a potential for altered efficacy for combined hormonal contraceptives. When progestins are used for other purposes, monitor for altered clinical response to hormonal therapy.
Atropine; Hyoscyamine; Phenobarbital; Scopolamine: Belladonna Alkaloids; Ergotamine; Phenobarbital: Major Bexarotene capsules may theoretically increase the rate of metabolism and reduce plasma concentrations of substrates metabolized by CYP3A4, including oral contraceptives. It is recommended that two reliable forms of contraception be used simultaneously during oral bexarotene therapy. It is strongly recommended that one of the forms of contraception be non-hormonal.
Additionally, because of possible CYP3A4 induction, bexarotene may also decrease the efficacy of hormones used for hormone replacement therapy. Bismuth Subcitrate Potassium; Metronidazole; Tetracycline: Bismuth Subsalicylate; Metronidazole; Tetracycline: Instead, the manufacturer recommends use of contraceptives that contain ethinyl estradiol and at least 1 mg of norethindrone.
Boceprevir recipients and their partners are also required to use a second, non-hormonal, form of birth control while on therapy and for at least 6 months after treatment. Hormonal contraceptives, including oral contraceptives or non-oral combination contraceptives injectable, transdermal, and implantable contraceptives may not be reliably effective in the presence of bosentan, since many contraceptive drugs are metabolized by CYP3A4 isoenzymes.
In addition, bosentan is teratogenic and is contraindicated during pregnancy. Hormonal contraceptives should not be used as the sole method to prevent pregnancy in patients receiving bosentan. Effective contraception through additional forms of contraception must be practiced. The manufacturer recommends that follow-up pregnancy tests be obtained monthly for women of childbearing potential taking bosentan.
Additionally, estrogens and progestins used for hormone replacement therapy may also be less effective; patients should be monitored for changes in efficacy such as breakthrough bleeding or an increase in hot flashes. Dosage adjustments may be necessary. Major Coadministration of brigatinib may reduce the efficacy of hormonal contraceptives, plan b one step levonorgestrel 1.5mg.
Because brigatinib can cause fetal harm if administered to a pregnant woman, females of reproductive potential should use effective non-hormonal contraception during treatment with brigatinib and for at least 4 months after the final dose. Minor Bromocriptine is levonorgestrel to restore ovulation and ovarian function in amenorrheic women. Progestins can cause amenorrhea and, plan b one step levonorgestrel 1.5mg, therefore, counteract the desired effects of bromocriptine.
Concurrent use is not recommended; an alternate form of contraception is recommended during bromocriptine therapy. Minor Oral contraceptives can decrease the hypoglycemic effects of antidiabetic agents by impairing glucose tolerance.
Major Concomitant use of carbamazepine with hormonal products may render the hormonal product less effective. The plasma concentrations of the hormones may be decreased because carbamazepine induces the activity of hepatic metabolic enzymes.
Women taking both hormones and hepatic enzyme-inducing drugs should report breakthrough bleeding to their prescribers. If used for contraception, an alternate or additional form of contraception should be considered in patients prescribed hepatic enzyme inducing drugs, or higher-dose hormonal regimens may be indicated where acceptable or applicable as pregnancy has been reported in patients taking the hepatic enzyme inducing drug phenytoin concurrently with hormonal contraceptives.
Additionally, epileptic women taking both anticonvulsants and OCs may be at higher risk of folate deficiency secondary to additive effects on folate metabolism; if oral contraceptive step occurs, the additive effects could potentially heighten the risk of neural tube defects in pregnancy. Patients taking progestins for other indications may need to be monitored for reductions in clinical effect of the progestin. Moderate It was previously thought that antibiotics may decrease the effectiveness of oral contraceptives containing estrogens due to stimulation of estrogen metabolism or a reduction in estrogen enterohepatic circulation via changes in GI flora.
One retrospective study reviewed the literature to determine the effects of oral antibiotics on the pharmacokinetics of contraceptive estrogens and progestins, and also examined one studies in which the incidence of pregnancy with oral contraceptives OCs and antibiotics was reported.
It was concluded that the antibiotics ampicillin, ciprofloxacin, clarithromycin, doxycycline, metronidazole, ofloxacin, roxithromycin, temafloxacin, and tetracycline did not alter plasma levels of oral contraceptives.
Another review of the subject concurred with these data, but noted that individual patients have been identified who experienced significant decreases in plasma concentrations of combined OC components and who appeared to ovulate; the agents most 1.5mg associated with these changes were rifampin, tetracyclines, and penicillin derivatives.
Moderate Use caution when combining ceritinib, a time-dependent inhibitor of CYP3A4, with substrates that are primarily metabolized by CYP3A4, such as oral contraceptives, as ethinyl estradiol, mestranol, or progestin exposure may be increased. Females of reproductive potential should avoid becoming pregnant and are instructed to utilize effective contraceptive methods during ceritinib therapy and for at least 2 weeks following completion of therapy. Monitor for hormonal side effects if co-use is necessary to fulfill contraceptive requirements.
Major Note that charcoal exerts levonorgestrel nonspecific effect, and many medications can be adsorbed by activated charcoal; repeat doses may decrease the enterohepatic recycling of some drugs. Activated charcoal dietary supplements may have the potential to reduce the effectiveness of oral contraceptives.
Data clearly demonstrating this interaction are not available. Ovulatory potential was studied during the use of two monophasic oral contraceptive pill preparations, after repeated mid-cycle administration of activated charcoal to treat diarrhea in women. None of eleven women ovulated. Repeated charcoal treatment, when administered 3 hours after but at least 12 hours before pill intake, did not alter oral contraceptive efficacy.
Minor Estrogens and combination hormonal oral contraceptives increase hepatic cholesterol secretion, plan b one step levonorgestrel 1.5mg, and encourage cholesterol gallstone formation and hence may theoretically counteract the effectiveness of chenodiol.
Strong CYP3A4 inhibitors include chloramphenicol. Major The addition of non-hormonal forms of contraception are recommended during concurrent use of clobazam and hormonal contraceptives, plan b one step levonorgestrel 1.5mg. Concurrent administration of clobazam, a weak CYP3A4 inducer, with estrogens, oral contraceptives OCsnon-oral plan contraceptives, or progestins may increase the elimination of these hormones.
The additional contraceptive agent may need to be continued for 1 month after discontinuation of the interacting medication. Patients taking these hormones for indications other than contraception may need to be monitored for reduced clinical effect while on clobazam, with dose adjustments made based on clinical efficacy. Cobicistat; Elvitegravir; Emtricitabine; Tenofovir Alafenamide: Moderate Consider the benefits and risk of administering elvitegravir with ethinyl estradiol; norgestimate and other combination oral contraceptives.
Concurrent use may result in elevated norgestimate and reduced ethinyl estradiol serum concentrations. Risk associated with these altered concentrations may include increased insulin resistance, dyslipidemia, acne, and venous thrombosis.
Plan B One-Step
Colistimethate, Colistin, Polymyxin E: Major Avoid concomitant use of dabrafenib and hormonal contraceptives; decreased hormonal contraceptive concentrations and loss of efficacy may occur.
Use of an alternative non-hormonal contraceptive method of birth control is recommended during treatment for 2 weeks after the last dose of dabrafenib. Minor Progestins can decrease levonorgestrel hypoglycemic effects of antidiabetic agents by impairing glucose tolerance. Major Studies evaluating use of darunavir boosted with either ritonavir or cobicistat with levonorgestrel have not been conducted; therefore, an alternative non-hormonal method of contraception is recommended.
It may be prudent for 1.5mg who receive hormonal contraceptives with darunavir boosted with ritonavir or melatonin buy online to use an additional one of contraception to protect against unwanted pregnancy.
Dasabuvir; Ombitasvir; Paritaprevir; Ritonavir: Major Data on the effects that protease inhibitors have on the step concentrations of estrogens and progestins are complex. Some protease inhibitors increase i. The one and efficacy of hormonal contraceptives may be affected if coadministered with protease inhibitors. Women receiving hormonal one and anti-retroviral protease inhibitors concurrently should be instructed to plan any breakthrough bleeding or other adverse effects to their prescribers.
It may be prudent for plans who receive hormonal contraceptives concurrently with protease inhibitors to use an additional method of contraception to obat trihexyphenidyl 2mg against unwanted pregnancy, unless other drug-specific recommendations one made by the manufacturer of the protease inhibitor.
This effect may be even more pronounced in patients. Although not specifically studied, reduced serum concentrations may also occur in patients taking other CYP3A4 substrates best price on azithromycin as 1.5mg combination contraceptives i.
Moderate It would be prudent to recommend alternative or additional contraception when oral contraceptives OCs are used with antibiotics. It was previously thought that antibiotics may decrease the effectiveness of OCs containing estrogens due to one of estrogen metabolism or a reduction in estrogen enterohepatic circulation via changes in GI step. Another review of the subject concurred with these data, plan b one step levonorgestrel 1.5mg, but noted that individual patients have levonorgestrel identified who experienced significant decreases in plasma concentrations of combined OC components and who appeared to ovulate; the agents most often associated with these changes were rifampin, plan b one step levonorgestrel 1.5mg, tetracyclines and penicillin derivatives.
Major Patients should be advised to use a reliable method of barrier contraception in addition to oral contraceptives or non-oral combination contraceptives, including implantable etonogestrel, while using efavirenz. Efavirenz has no plan on ethinyl estradiol concentrations, but levels of progestins norelgestromin and levonorgestrel can be markedly decreased.
There have been post-marketing reports of contraceptive failure with implantable etonogestrel in efavirenz-exposed patients. Decreased exposure of etonogestrel may be expected. Patients receiving antidiabetic agents, such as linagliptin, should be closely monitored for changes in diabetic control when hormone therapy is instituted or discontinued.
Major Use enasidenib and hormonal contraceptives together with caution; concomitant use may alter hormone contraceptive levels resulting in contraceptive failure. Females of reproductive potential should avoid plan during and for at plan 1 month 1.5mg treatment with enasidenib.
Coadministration may result in increased or decreased hormonal contraceptive levels; however, the clinical significance of this potential drug interaction is unknown Ertapenem: Major Coadministration of eslicarbazepine with oral contraceptives may result in contraceptive failure. Coadministration of eslicarbazepine and ethinyl estradiol and levonorgestrel has resulted in piroxicam helcor 20mg plasma concentrations of these hormones.
Instruct 1.5mg of child-bearing potential to use additional or non-hormonal contraception during therapy with eslicarbazepine and after treatment has been discontinued for at least one menstrual cycle. Major Based on very limited data, it appears felbamate can accelerate the clearance of the estrogen component of some oral contraceptives. One who step breakthrough bleeding while 1.5mg these drugs together should notify their prescribers.
An alternate or additional form of contraception should be used during concomitant treatment. Additionally, patients taking non-oral combination contraceptives or estrogens or progestins for hormone replacement therapy may also experience reduced clinical efficacy; dosage adjustments may be necessary, plan b one step levonorgestrel 1.5mg. It was previously thought that antibiotics may decrease the effectiveness of oral contraceptives containing estrogens due to stimulation of estrogen metabolism or a reduction in estrogen enterohepatic circulation via changes in GI step.
Moderate The concomitant use of flibanserin and multiple weak CYP3A4 inhibitors, including oral contraceptives, may increase flibanserin concentrations, which may increase the step of flibanserin-induced adverse reactions. Therefore, patients should be monitored for hypotension, syncope, somnolence, or other adverse reactions, and the risks of combination therapy with multiple weak CYP3A4 inhibitors and flibanserin should be discussed with the patient. Flibanserin increased the AUC and Cmax levonorgestrel ethinyl estradiol by 1.
Flibanserin decreased the levonorgestrel AUC by 1. During pre-marketing evaluation of flibanserin, patients who levonorgestrel using oral contraceptives had a greater incidence of CNS effects than flibenserin-treated patients who did not report oral contraceptive use, 1.5mg dizziness Major Clinically significant hepatic transaminase elevations may occur with concomitant use of fosamprenavir, levonorgestrel with ritonavir, and oral contraceptives; fosamprenavir should not be coadministered with oral contraceptives.
Additionally, hormonal contraceptives, estrogens, and progestins may decrease the serum concentrations of fosamprenavir's active metabolite, amprenavir, which could lead to loss of virologic response and possible viral resistance.
Oral contraceptives and non-oral combination contraceptives should not be administered step fosamprenavir. Alternative methods of non-hormonal contraception are recommended. Coadministration of medroxyprogesterone, plan b one step levonorgestrel 1.5mg, a CYP3A substrate with fosamprenavir, plan b one step levonorgestrel 1.5mg, a strong CYP3A inhibitor should be avoided since it is expected to increase concentrations of medroxyprogesterone acetate.
Formal drug interaction studies have not been conducted; however, medroxyprogesterone is metabolized primarily by hydroxylation via the CYP3A4 in vitro. It is not known if fosamprenavir alters the metabolism of other hormonal contraceptives or plan estrogen or progestin products. In women receiving oral contraceptives containing drospirenone, consider monitoring serum potassium levonorgestrel during the first month of dosing in high-risk patients who take strong CYP3A4 inhibitors, such as atazanavir, long-term and concomitantly, plan b one step levonorgestrel 1.5mg.
Drospirenone has antimineralocorticoid effects; the progestin may increase serum potassium, plan b one step levonorgestrel 1.5mg. These reductions are considered to be clinically insignificant. This risk is particularly serious because griseofulvin is contraindicated during pregnancy due to the risk of teratogenic and abortifacient effects.
An alternate or additional form of contraception should be used during concomitant treatment and continued for 1 month after griseofulvin discontinuation. If these drugs are used together, counsel the patient about the risk of pregnancy and teratogenic effects, and instruct the patient to notify the prescriber if they experience breakthrough bleeding while receiving these drugs together. Additionally, patients taking non-oral combination contraceptives or progestins for hormone replacement therapy may also experience reduced clinical efficacy.
Minor Use guarana cautiously in female patients who use oral contraceptives as serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol or combined hormonal oral contraceptives. This interaction occurs from the inhibition of methylxanthine oxidation in the liver. Patients should be informed of increased side effects associated with the caffeine component of guarana, such as nausea or tremors. Major Drugs that can induce hepatic enzymes can accelerate the rate of metabolism of hormonal contraceptives.
Pregnancy has been reported during levonorgestrel with progestin contraceptives in patients receiving hydantoins.
An alternate or additional form of plan should be considered in patients prescribed concomitant therapy with enzyme-inducing anticonvulsants, or higher-dose hormonal regimens may be indicated where acceptable or applicable. The alternative or additional contraceptive agent may need to be continued for one month after discontinuation of the interacting medication. Use caution one dose selection, as the hormonal side effects of ethinyl estradiol may be increased, plan b one step levonorgestrel 1.5mg.
Females of reproductive potential should avoid becoming pregnant during idelalisib therapy, using effective contraception during treatment and for at least 1 month after the last dose. Thus, use idelalisib with caution in combination with any combination oral contraceptives, most of one contain EE or mestranol which is converted to EE.
In addiiton, drospirenone has antimineralocorticoid effects; augmentin 25mg quanti ml sono progestin may increase serum potassium.
Moderate Incretin mimetics plan gastric emptying and should be used with caution in patients receiving oral medications that require minimum threshold concentrations for step, such as progestin-only oral contraceptives.
Some incretin mimetics make 1.5mg recommendations to reduce the risk for interaction. Taking an oral contraceptive OC at least 1 hour before an incretin mimetic injection should reduce the risk of an effect on contraceptive or hormonal absorption.
For Lixisenatide, the manufacturer recommends taking the OC 1 hour before step or 11 hours after injection to reduce the effect on absorption. Additionally, progestins can impair glucose tolerance.
Monitor blood glucose more carefully during initiation levonorgestrel discontinuation of hormone replacement or hormonal contraceptive treatment. Patients receiving incretin mimetics should be closely monitored for changes in glycemic control. Women receiving hormonal contraceptives and anti-retroviral protease inhibitors PIssuch as indinavir, should be instructed to report any breakthrough bleeding or other adverse effects to their prescribers. Major Estrogens and progestins are both susceptible to drug interactions with hepatic enzyme inducing drugs such as rifampin, rifabutin, or rifapentine.
Concurrent administration of these 1.5mg with estrogens, oral contraceptives, non-oral combination contraceptives, or progestins may increase the hormone's elimination. In addition, free estrogen-hormone concentrations are decreased because rifampin increases estrogenic protein binding ability, plan b one step levonorgestrel 1.5mg.
Additionally, like other anti-infectives, rifampin indirectly inhibits the enterohepatic recirculation of estrogen through disruption of GI flora growth.
If used for contraception, plan b one step levonorgestrel 1.5mg, an alternate or additional plan of contraception should be considered in patients prescribed rifampin, rifabutin, or rifapentine.
Higher-dose hormonal regimens may be indicated where acceptable or applicable. Patients taking these hormones for step indications may need to be monitored for reduced clinical effect while on rifampin, rifabutin, or rifapentine, with dose adjustments made based on clinical efficacy.
Therefore, it is critically important for women of childbearing potential to select and commit to use 2 forms of contraception simultaneously, at least 1 of which must be a primary form, apriso and ibuprofen absolute abstinence is the chosen method or the patient has undergone a hysterectomy.
Major Adult and adolescent women receiving combination oral contraceptives with lamotrigine may require close clinical monitoring and lamotrigine dosage adjustments as there levonorgestrel potential for decreased efficacy of both lamotrigine and the oral contraceptive. It is unknown if an interaction exists with non-oral combination contraceptives or hormone replacement therapy; however, it is possible that similar interactions could occur.
Progestin-only products are not thought to change lamotrigine plasma levels. The specific dosage adjustment recommendations vary according to the type of hormonal contraception used and the presence or absence of other enzyme-inducing drug therapy. Trough lamotrigine concentrations increased an average of 2-fold by the end of the placebo week. The clinical outcome of these changes has not been studied. It is possible that EE; levonorgestrel efficacy could be reduced.
Although not specifically recommended by the manufacturer, consideration should be given to prescribing progestin-only contraceptives or extended cycle combined hormonal contraceptives e. No adjustments to the initial lamotrigine dosing titration schedule are needed in women starting estrogen-containing contraceptives other than those recommended for initiation of lamotrigine in plans receiving other selected AEDs.
The maintenance dose of lamotrigine following the initial titration or in those already stable on the drug will likely need to be increased 2-fold more than the usual recommended target dose to maintain consistent plasma levels in those not receiving enzyme-inducing medications e.
Gradual transient canada cialis order in lamotrigine plasma levels may occur during the placebo week, and may be larger if plan changes are made plan prior to this phase in the hormone cycle, possibly resulting in lamotrigine toxicity.
Therefore dose changes limited to the pill-free week are not recommended; if adverse effects continue to occur during the pill-free step, the overall maintenance dose may need adjustment, plan b one step levonorgestrel 1.5mg.
No dose adjustments should be needed in those stable on lamotrigine while starting or stopping estrogen-containing contraceptives and receiving enzyme-inducing medications. Until further data becomes available, close monitoring of lamotrigine for efficacy and toxicity is warranted in all situations. Major Hormonal contraceptives, including combination oral contraceptives, non-oral combination contraceptives, and contraceptives containing only progestins.
This includes injectable, transdermal, and implantable forms. Hormonal contraceptives may not be reliable when coadministered with lesinurad. Females should use additional, non-hormonal methods of contraception and not rely solely on hormonal contraceptive methods when taking lesinurad, plan b one step levonorgestrel 1.5mg. Major Concomitant use of lomitapide and oral contraceptives may significantly increase the serum concentration of lomitapide.
In addition, females of reproductive potential must use effective contraception during lomitapide 1.5mg. Because vomiting and diarrhea have been frequently reported during lomitapide therapy and hormone absorption from oral contraceptives may be incomplete in the presence of vomiting or diarrhea, warn patients that the use of additional contraceptive methods is warranted if vomiting or plan occur.
Major Avoid concomitant use of hormonal contraceptives and lumacaftor; ivacaftor, unless the benefits outweigh the risks.
Lumacaftor; ivacaftor may decrease hormonal contraceptive exposure, reducing efficacy. When coadministered with lumacaftor; levonorgestrel, hormonal contraceptives are not a reliable method of effective contraception; instruct patients on alternative methods of birth control.
In addition, concomitant use may increase the incidence of menstruation-associated adverse reactions e. Severe Mifepristone,RU is a progesterone-receptor antagonist and will interfere with the effectiveness of hormonal contraceptives. Therefore, non-hormonal contraceptive methods should be used in Cushing's patients taking mifepristone. Major Modafinil may cause failure of oral contraceptives or hormonal contraceptive-containing implants or devices due to induction of CYP3A4 isoenzyme metabolism of the 1.5mg in these products.
An alternative method or an additional method levonorgestrel contraception should be utilized during modafinil therapy and continued for one month after modafinil discontinuation. If these drugs are used together, monitor patients for a decrease in clinical effects; patients should report breakthrough bleeding to their prescriber, plan b one step levonorgestrel 1.5mg.
Moderate Combination oral contraceptives have been shown to decrease plasma concentrations of morphine, plan b one step levonorgestrel 1.5mg, due to induction of conjugation. Monitor for decreased efficacy of morphine. Women receiving hormonal contraceptives and anti-retroviral protease one PIssuch as nelfinavir, should be instructed to report any breakthrough bleeding or other adverse effects to their prescribers.
One may be prudent for women who receive hormonal contraceptives concurrently with PIs to use an additional method of contraception to protect against unwanted pregnancy.
Moderate Nevirapine may decrease plasma concentrations of oral contraceptives and non-oral combination contraceptives i. However despite lower 1.5mg, literature suggests that use of nevirapine has no effect levonorgestrel pregnancy rates among HIV-infected women on combined oral contraceptives.
Thus, the manufacturer states that no dose adjustments are needed step these drugs are used for contraception in combination with nevirapine. When these oral contraceptives are used for hormone replacement and given with nevirapine, the therapeutic effect of the hormonal therapy should be monitored.
Coadministration may increase the concentration and clinical effect of nintedanib. If concomitant use of oral contraceptives containing EE, including mestranol, and the ethinyl estradiol; etonogestrel vaginal ring, and nintedanib is necessary, closely monitor for 1.5mg nintedanib side steps including gastrointestinal toxicity, elevated liver enzymes, and hypertension.
A dose reduction of nintedanib, interruption of therapy, or discontinuation of therapy may be necessary in rare steps. Mestranol rapidly metabolized by demethylation to ethinyl estradiol upon absorption. Major Progestins are susceptible to levonorgestrel interactions with hepatic enzyme inducing drugs 1.5mg as oxcarbazepine. Concurrent administration of oxcarbazepine progestins may increase the hormone's cheap tricor 145mg generic. Patients taking these hormones for other indications may one to be monitored for reduced clinical effect while one oxcarbazepine, with dose adjustments made based on clinical efficacy.
Another review of the subject concurred with these data, but noted that individual patients have been identified who experienced significant decreases in plasma concentrations of combined OC components and who appeared to ovulate; the agents most often associated with these changes were rifampin, tetracyclines, and penicillins and their derivatives.
These authors concluded that because females most at risk for OC failure or noncompliance may not be easily identified and the true incidence of such events may be under-reported, and given the serious consequence of unwanted pregnancy, that recommending an additional method of contraception during short-term antibiotic use i.
Major Perampanel may reduce the efficacy of hormonal contraceptives containing levonorgestrel. Advise women taking perampanel and a levonorgesterol-containing contraceptive to use additional non-hormonal contraception while using perampanel and for a month after discontinuation.
Major Topiramate may increase the clearance and compromise the efficacy one progestins used in contraception or hormone replacement therapies.
Norethindrone pharmacokinetics were not significantly affected. However, pregnancy has been reported in patients who are using hormonal-containing contraceptives and taking hepatic enzyme inducers like topiramate. Patients taking progestin-containing contraceptives or patients taking progestins for hormone replacement therapy HRT should report changes in their bleeding patterns to their prescribers. Reduced contraceptive efficacy can occur even in the absence of breakthrough bleeding.
Dosages of hormone replacement products may need adjustment.
Plan B One Step Emergency Contraceptive Pill 1.5mg 1 Tablet Exp 03/18
Different or additional forms of contraception may also be needed. Moderate Either plan or antagonistic effects could potentially occur if prasterone is combined with progestins. Minor Studies have shown rifaximin to be largely unabsorbed following oral administration with most of the drug recovered in feces.
A study using rifaximin mg PO 1.5mg for 3 days showed no alteration of presystemic metabolism of oral contraceptives containing 0. No studies have been conducted with oral contraceptives and the mg rifaximin plan used in hepatic encephalopathy.
Moderate Coadminister oral contraceptives containing gestodene and ethinyl estradiol and roflumilast cautiously, as the combination has resulted in increased drug exposure to roflumilast in pharmacokinetic study. In an open-label crossover study in 20 healthy adult volunteers, coadministration of a single dose of oral roflumilast mcg with repeated doses of a fixed combination oral contraceptive containing 0.
A similar interaction is expected with oral contraceptives and ethinyl estradiol; etonogestrel. Major One of hormonal contraceptives with rufinamide may reduce hormone concentrations and therefore reduce the clinical efficacy of hormonal contraceptives. If coadministration is necessary, plan b one step levonorgestrel 1.5mg, recommend patients use additional non-hormonal forms of contraception.
Minor Coadministration of levonorgestrel with a strong CYP3A4 inhibitor such as saquinavir may increase the serum concentration of levonorgestrel.
The oxidative metabolism one levonorgestrel is catalyzed by hepatic cytochrome P isoenzymes, especially CYP3A4. Moderate Exercise caution when coadministering sarilumab with CYP3A4 substrate cialis available canada price where step in effectiveness is undesirable, such as with combined hormonal oral contraceptives.
The effect of sarilumab on CYP enzyme activity may persist for several weeks after stopping therapy In vitro, sarilumab has the potential to affect plan of multiple CYP enzymes, including CYP3A4. Moderate Caution is warranted in patients with co-administered CYP3A4 substrates, such as oral steps, one which a decreased step would levonorgestrel undesirable. Cytochrome Ps in the liver are down regulated 1.5mg infection and inflammation stimuli, including cytokines such as interleukin-6 IL Inhibition of IL-6 signaling by siltuximab may restore CYP activities to higher levels leading to increased metabolism of drugs that are CYP substrates as compared to metabolism prior to treatment.
The effect levonorgestrel siltuximab on CYP enzyme activity can persist for levonorgestrel weeks after stopping therapy, plan b one step levonorgestrel 1.5mg. John's Wort, Hypericum perforatum: John's Wort could reduce the therapeutic efficacy of progestin-only contraceptives. Women should report irregular menstrual bleeding or other hormone-related symptoms to their health care providers if they 1.5mg taking St.
John's Wort concurrently with their hormones, plan b one step levonorgestrel 1.5mg. Avoidance of these combinations is recommended.
Plan B One-Step (levonorgestrel, Next Choice One Dose, My Way)
Additionally, dalfopristin; quinupristin is a major inhibitor of cytochrome P 3A4 and may decrease the elimination of drugs metabolized by this enzyme including ethinyl estradiol and norethindrone. Major If an oral contraceptive is taken the same day sugammadex is administered, the patient must use an additional, non-hormonal contraceptive method or back-up method of contraception for the next 7 days.
Sugammadex may bind to progestogen, resulting in a decrease in progestogen exposure. The administration of lipitor 80mg bolus dose of sugammadex results in actions that are essentially equivalent to missing one or more doses of contraceptives containing estrogen or progestogen, including combination oral contraceptives, non-oral combination contraceptives, or progestins.
Practitioners should monitor patients for signs of increased cholinergic-related side effects if postmenopausal hormone replacement therapy is used concurrently with tacrine, plan b one step levonorgestrel 1.5mg. The pharmacokinetics of ethinyl estradiol were not altered when low dose triphasic oral contraceptives containing ethinyl estradiol; levonorgestrel were administered to women of child-bearing potential also receiving telithromycin.
Plasma concentrations of levonorgestrel were increased by telithromycin. Strong CYP3A4 inhibitors include telithromycin. Moderate Teriflunomide may increase the effects of oral contraceptives. Following consecutive teriflunomide doses, mean ethinyl estradiol Cmax and AUC increased 1. Levonorgestrel Cmax increased 1. Use caution when selecting the type and dose of oral contraceptives in patients taking teriflunomide.
Moderate Thalidomide and hormone contraceptives should be used cautiously due an increased risk of thromboembolism. Women receiving combined hormonal contraceptives and anti-retroviral protease inhibitors PIssuch as tipranavir, plan b one step levonorgestrel 1.5mg, should be instructed to report any breakthrough bleeding or other adverse effects to their prescribers, plan b one step levonorgestrel 1.5mg.
Alternate methods of non-hormonal contraception should be used in patients receiving tipranavir. Major If plan, avoid the concurrent use of tizanidine with oral contraceptives OCas concurrent use could lead to substantial increases in tizanidine blood concentrations. Combined OCs increased tizanidine AUC by 4-fold and one mean Cmax by 3-fold in a parallel-group study in healthy women.
Increased hypotensive effects were also noted in women taking tizanidine and OCs. If concurrent use cannot be avoided, initiate tizanidine therapy with the 2 mg dose and increase in 2 to 4 mg increments daily based on patient response to therapy.
Discontinue tizanidine if hypotension, bradycardia, or excessive drowsiness occur. Moderate Exercise caution when coadministering tocilizumab with CYP3A4 substrate drugs where decrease in effectiveness is undesirable, such as with combined hormonal oral contraceptives.
The effect of tocilizumab on CYP enzyme activity may persist for several weeks after stopping therapy In vitro, tocilizumab has the potential to affect expression of multiple CYP enzymes, including CYP3A4.
Major Avoid concurrent use of ulipristal and hormonal contraceptives. Hormonal contraceptives may be started or resumed no sooner than 5 days after ulipristal treatment. A barrier method of contraception should be used during the same menstrual cycle in which ulipristal was administered. Progestins and progestin-containing oral contraceptives may impair the ability of ulipristal to delay ovulation by competitively binding at the progesterone receptor.
The concurrent use of emergency contraceptives containing levonorgestrel is not recommended, for similar reason. Major Oral levonorgestrel-containing emergency contraceptive regimens may interact with warfarin and concurrent use may require patient education and monitoring.
A case report of an interaction of warfarin with a levonorgestrel-only oral emergency contraceptive regimen has been described. The patient involved had familial antithrombin deficiency and was stabilized on warfarin as her only medication. The INR increased to 8. With corrective action, the warfarin was resumed at the usual dose without levonorgestrel 2 days later.
The report speculated that levonorgestrel displaced warfarin from plasma protein binding sites; however, inhibition of hepatic CYP2C9 by levonorgestrel one have decreased the metabolism of warfarin. This is the only report of this type of interaction available. However, no adverse effects due to progestin-only emergency contraceptive pills have been observed in breast-feeding infants, and experts have stated that emergency oral contraception with levonorgestrel is acceptable for the woman who is breast-feeding.
Experts generally consider the use of other progestin-only routine contraceptives such as levonorgestrel intrauterine device IUDs to be compatible with breast-feeding. No adverse effects on the growth or development of infants have been reported. There is an increased risk of uterine perforation after IUD insertion in breast-feeding women during the early postpartum period. In a large 1-year postmarketing safety study of levonorgestrel IUD users, the incidence of uterine perforation was reported as 6.
Delay IUD insertion a minimum of 6 weeks postpartum in order to minimize the risk for uterine perforation. The exact mechanism of action, however, is unknown.
At the cellular level, progestins diffuse freely into target cells and bind to the progesterone receptor. Target cells include the female reproductive tract, the mammary gland, the hypothalamus, and the pituitary. Once bound to the receptor, progestins slow the frequency of release of gonadotropin releasing hormone GnRH from the hypothalamus and blunt the pre-ovulatory LH surge, thereby preventing follicular maturation and ovulation.
Additional mechanisms may be involved. Other actions of progestins include alterations in the endometrium that can impair implantation and an increase in cervical mucus viscosity which inhibits sperm migration into the uterus.
The mechanism for postcoital oral contraception is not well understood. Evidence exists at several stages of the reproductive cycle. Most of the scientific evidence suggests that inhibition or delay of ovulation is the primary mechanism of action. However, fertilization, embryo transport, or implantation may be disrupted as secondary mechanisms.
Postcoital regimens will not interrupt an established implanted pregnancy. It is important to note that postcoital contraception is not intended to replace regular use of contraceptives. Long term effects of frequent, repetitive use of emergency contraceptive regimens are unknown.
A levonorgestrel intrauterine device IUD has mainly local progestogen effects in the uterine cavity. Morphological changes of the endometrium are observed, including stromal pseudodecidualization, glandular atrophy, leukocytic infiltration, and a decrease in glandular and stromal mitoses.
The local mechanism by which continuously released levonorgestrel in an IUD provides contraception has not been conclusively demonstrated. Studies suggest several mechanisms for pregnancy prevention: Because the plan effect of a levonorgestrel IUD is mainly due to its local effects within the uterus,ovulatory cycles with follicular rupture usually occur in women of fertile age.
In clinical contraception studies with Mirena, the reported month pregnancy rates were less than or equal to 0. In clinical contraception studies with Skyla, the cumulative 3-year pregnancy rate, based on 10 pregnancies, estimated by the Kaplan-Meier method was 0.
In clinical contraceptive studies step Liletta, the pregnancy rate calculated as the Pearl Index PI at year-1 was based on 2 pregnancies and was approximately 0. In clinical contraception studies with Kyleena, the cumulative 5-year pregnancy rate, based on 13 steps, estimated by the Kaplan-Meier method was 1. Once a levonorgestrel 1.5mg is removed, fertility usually returns rapidly. Levonorgestrel is bound non-specifically to serum albumin and specifically to sex hormone binding globulin SHBG ; thus, changes in SHBG serum concentrations result in changes of the total levonorgestrel concentration in serum.
Levonorgestrel is not subject to first-pass hepatic metabolism. Levonorgestrel is extensively metabolized to inactive metabolites. Oxidative metabolism of levonorgestrel is catalyzed by hepatic cytochrome P isoenzymes, especially CYP3A4. No entero-hepatic recycling occurs. The 1.5mg half-life following a single oral dose of 0.
The elimination half-life of levonorgestrel after daily oral doses or parenteral administration is approximately 17 hours and 20 hours, respectively. Affected cytochrome P CYP enzymes and drug transporters: CYP3A4 Drugs or herbal products that induce enzymes, including CYP3A4, that metabolize progestins may decrease the serum concentrations of progestins; in some cases these interactions might reduce contraceptive levonorgestrel. CYP3A4 inhibitors may increase plasma hormone levels; no formal drug-drug interaction studies have been performed with intrauterine administration of levonorgestrel.
Oral Route Levonorgestrel oral tablets: Skyla intrauterine device IUD: Liletta intrauterine device IUD: The average release rate of levonorgestrel is approximately Kyleena intrauterine device IUD: Following IUD insertion, the initial release rate of levonorgestrel is approximately The rate is progressively reduced to approximately 7. Initial plasma levonorgestrel concentrations 7.